Humanizing Healthcare #healthequity
- Rebekon Consulting LLC
- Jul 11, 2024
- 12 min read
Updated: Sep 12, 2024
Humanizing the Healthcare Ecosystem for Trans, Gender Diverse and Intersex patients #healthequity
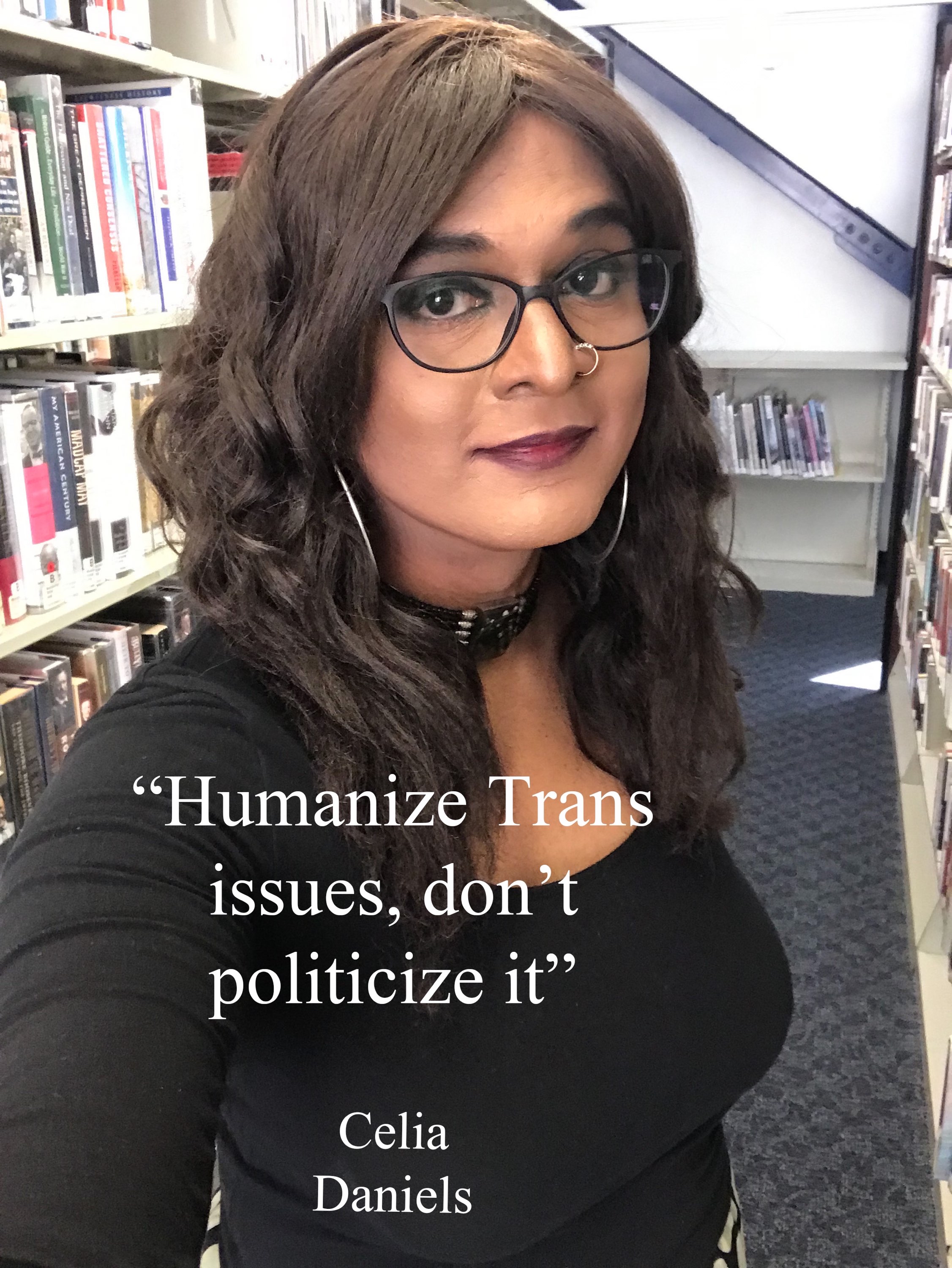
by Celia Sandhya Daniels
Racial, Sexual and Gender minority continue to face healthcare challenges.
Several years ago, during a routine exam, I informed my doctor about my gender incongruence. He felt awkward and asked several questions that clearly showed he did not understand my experience. One in five transgender individuals end up educating their doctors about gender incongruence and its symptoms. While I was explaining that gender incongruence can cause suicidal ideation, self-harm, anxiety, low self-esteem, and depression, he fixated on suicidal ideation and called the nurse to address my suicidal thoughts. I explained to the nurse that I have a supportive family and am not suicidal. I also told her that listening to patients rather than making assumptions is crucial.
The trans, gender diverse and intersex (TGI) community continues to face numerous challenges when it comes to accessing quality healthcare. Especially within the four pillars of the healthcare ecosystem. This is due to a lack of knowledge and understanding among healthcare providers, systemic discrimination and biases, and a lack of legal protections. As a result, transgender individuals experience significant health disparities and poorer health outcomes than the general population. Achieving healthcare equity for transgender people requires a multifaceted approach that addresses these barriers at every level.
Based on ACLU, more than hundred bills seeking to restrict transgender healthcare access have been introduced across various states beginning in early 2023. Bills targeting other facets of trans livelihood have been filed in many of the same states and are expected in several others with GOP majorities.
Gender-affirming healthcare providers and parents of trans youths are the primary targets of these bills, many of which seek to criminalize helping a trans child obtain what doctors and psychologists widely consider “medically necessary care.”
Four Pillar of the Healthcare ecosystem
Bottomline, if you want to create a change in the healthcare ecosystem, we need to focus on the "4Ps" or Four Pillar in the healthcare ecosystem - The Providers, Payers, Pharmaceutical companies and Policy Makers

The Four Pillars of the Healthcare Ecosystem - (c) Rebekon Consulting LLC
First Pillar: Providers

Nearly one-third of transgender individuals report being refused medical care or harassed by healthcare providers due to their gender identity. This mistreatment can lead to a quarter of transgender people avoiding medical visits altogether.
Transgender discrimination by healthcare providers is a significant barrier to accessing quality healthcare for transgender individuals. Medical providers often have a poor understanding of intersex communities due to limited training and awareness. Intersex individuals, who are born with sex characteristics that do not fit typical definitions of male or female, frequently face medical professionals who lack knowledge about their unique health needs. This can lead to inappropriate treatments, misdiagnoses, and a lack of sensitive, patient-centered care. Improving medical education on intersex issues is crucial to ensure that intersex patients receive the respectful and competent healthcare they deserve.
Discrimination can manifest in several ways, including:
Lack of knowledge and training: Healthcare providers may lack knowledge and training about transgender health issues, which can lead to delays in care, inadequate treatment, and a lack of access to preventative care.
Bias and prejudice: Healthcare providers may hold biases and prejudices against transgender individuals, which can lead to discrimination and mistreatment. For example, a provider may refuse to use a transgender individual's preferred name or pronouns or deny them access to gender-affirming care.
Stereotyping: Providers may stereotype transgender individuals, assuming that they are all the same and are only seeking care related to their gender identity. This can lead to a lack of attention to other health concerns or a lack of understanding of the individual's unique needs.
Lack of privacy and confidentiality: Transgender individuals may fear discrimination or harm if their gender identity is revealed. They are outed without their consent. Healthcare providers may inadvertently or intentionally breach confidentiality, leading to a loss of trust and a reluctance to seek care.
Denial of care: Some healthcare providers may refuse to provide care to transgender individuals based on their gender identity, violating their legal right to access healthcare without discrimination.
I have been outed many times in the doctor's office because they recorded my authentic name and pronouns in the notes section instead of alongside my legal name and gender at birth. This practice has led to my privacy being compromised, as my authentic identity was not integrated into my main medical records, resulting in unintentional disclosure of my transgender status. It is crucial for medical providers to properly document and respect the identities of transgender patients to ensure their privacy and dignity are maintained.
Education and Training for Healthcare Providers
One of the most significant barriers to healthcare equity for transgender individuals is a lack of knowledge and understanding among healthcare providers. Medical providers typically receive no or only 5-6 hours of training on LGBTQ+ issues, which is insufficient. Transgender individuals often encounter providers who are not trained to care for their unique needs, leading to delays in care, inadequate treatment, and a lack of access to preventative care. Therefore, it is crucial to provide education and training for healthcare providers to address this knowledge gap. Training should cover topics such as gender identity, hormone therapy, and surgical options, as well as how to create a welcoming and affirming environment for transgender patients. By increasing the knowledge and competency of healthcare providers, transgender individuals can receive the care they need without fear of discrimination.
Creating Inclusive Policies and Guidelines
Another critical step in achieving healthcare equity for transgender individuals is creating policies and guidelines that promote inclusive care. Healthcare facilities should adopt non-discrimination policies that specifically include gender identity and expression. In addition, facilities should establish protocols for providing transgender-specific care, such as hormone therapy and surgical options. These policies and guidelines should be developed in collaboration with transgender individuals to ensure they meet the unique needs of the community.
Legal Protections
Legal protections are essential for ensuring healthcare equity for transgender individuals. Transgender individuals are currently not protected under federal law, and many states do not have legal protections for transgender individuals in healthcare settings. Laws and regulations should be updated to protect transgender individuals from discrimination in healthcare, including denying access to care, refusing treatment, and insurance exclusions.
Access to gender-affirming care
Access to gender-affirming care, such as hormone therapy and surgical options, is essential for the health and well-being of transgender individuals. Healthcare providers should provide these options when appropriate, and insurance companies should cover the costs of these services. Additionally, there should be efforts to increase the availability of gender-affirming care in areas where it is not currently available
Community Outreach and Advocacy
Creating a supportive community is vital to improving healthcare equity for transgender individuals. Community-based organizations can provide critical support to transgender individuals, including access to healthcare, legal resources, and support groups. These organizations can also advocate for policy changes and provide education and training to healthcare providers. By building a supportive community, transgender individuals can access the resources and care they need to improve their health outcomes.
The World Professional Association for Transgender Health said last year that teens experiencing gender dysphoria can start taking hormones at age 14 and can have certain surgeries at ages 15 or 17. The group acknowledged potential risks but said it was unethical to withhold early treatments, which can improve psychological well-being and reduce suicide risk.
Healthcare equity for transgender individuals requires a comprehensive approach that addresses the barriers faced by the community. By providing education and training to healthcare providers, creating inclusive policies and guidelines, enacting legal protections, and building a supportive community, we can ensure that transgender individuals receive quality healthcare without discrimination or bias. Achieving healthcare equity for transgender individuals is not only a human rights issue but a public health imperative. It is time to break down the barriers and ensure that all individuals, regardless of their gender identity, have access to equitable and affirming healthcare.
Second Pillar: Payers

I have faced several insurance claim denials because the insurance company adjusted my policy based on my sex at birth instead of how I identify currently. Transgender individuals can face discrimination from insurance companies, which can limit their access to essential healthcare services. This discrimination can take various forms, including:
Coverage Exclusions: Some health plans still use exclusions that deny coverage for “services related to sex change” or “sex reassignment surgery.” These exclusions can prevent transgender individuals from accessing necessary healthcare services.
Exclusion of gender-affirming care: Insurance companies may refuse to cover gender-affirming care, such as hormone therapy or gender confirmation surgery, or may place unnecessary obstacles in the way of receiving these treatments.
Denial of coverage: Insurance companies may deny coverage for medical services based on a transgender person's gender identity, or require excessive documentation to "prove" their gender identity or medical necessity.
Varying Policies: Coverage varies by state and insurance carrier. While most insurers have eliminated transgender-specific exclusions, it’s essential to review the complete terms of coverage before enrolling in a plan
Name and Gender Matching: When applying for Marketplace coverage, transgender individuals should use the name on their Social Security card and select the sex consistent with other legal documents. Some state Medicaid agencies may verify sex against available records.
Limited coverage: Even when insurance companies do provide coverage for gender-affirming care, coverage may be limited or inadequate, leading to financial burdens and reduced access to care.
Justification hurdles: Trans patients may need to jump through more hoops to get approval for procedures, including letters from therapists documenting medical necessity.
To address discrimination by insurance companies, several steps can be taken. These include:
Preventive Services: Health plans must cover sex-specific preventive services without discrimination based on sex assigned at birth or gender identity. For example, a transgender man needing a mammogram or pap smear should receive coverage.
Legal protections: Transgender individuals should have legal protections from insurance discrimination, such as bans on discriminatory exclusions, and clear guidance on providing gender-affirming care.
Advocacy: Transgender individuals and their allies can advocate for changes in insurance policies, such as lobbying for broader coverage for gender-affirming care. If denied coverage, individuals have appeal options to challenge insurance decisions.
Insurance plan research: Transgender individuals should research insurance plans carefully to find ones that provide coverage for gender-affirming care and ensure that the policy is free of discriminatory practices.
Financial assistance: Transgender individuals may benefit from financial assistance programs, such as grants or loans, that can help cover the cost of medical treatments.
Healthcare provider support: Healthcare providers can support transgender individuals by providing documentation and advocacy to help secure insurance coverage for gender-affirming care.
Federal and State Law: The Affordable Care Act protects against discrimination based on sex, which may include transgender health care.Many states have laws that specifically prohibit insurers from excluding transgender care.
Overall, transgender discrimination by insurance companies is a significant barrier to accessing quality healthcare for transgender individuals. To address this issue, legal protections must be established, advocacy efforts should be undertaken, insurance plan research and financial assistance may be needed, and healthcare providers should support transgender individuals in obtaining the coverage they need. These efforts can ensure that transgender individuals receive the care they need without fear of discrimination or bias from insurance companies.
Third Pillar: Pharmaceuticals and Clinical Trials
Transgender individuals often face discrimination in clinical trials, which can limit their access to potentially life-saving treatments and further perpetuate health disparities. Discrimination can manifest in several ways, including:
Exclusion from trials: Transgender individuals may be excluded from clinical trials due to their gender identity or due to their use of hormone therapy. Most trials rely on a binary system for sex (male/female) in recruitment and data collection, excluding TGI identities.
Limited data: Clinical trials may not collect or report data on gender identity, leading to a lack of understanding of the efficacy and safety of treatments for transgender individuals.
Misgendering: Researchers or healthcare providers may misgender or use the wrong pronouns for transgender individuals in clinical trials, leading to a lack of comfort, and trust, and potentially impacting their willingness to participate.
Insufficient healthcare: Clinical trial protocols may not account for the specific healthcare needs of transgender individuals, leading to adverse health outcomes or high drop-out rates.
Distrust in Healthcare: Negative experiences with healthcare providers can lead to distrust and a reluctance to participate in research.
Confidentiality Concerns: TGI individuals might worry about their gender identity being revealed during the trial
I participated in a cardiovascular clinical trial to make a difference in how my data is collected as a gender nonbinary patient.
To address transgender discrimination in clinical trials, several steps can be taken:
Inclusion of transgender individuals: Clinical trials should include transgender individuals to ensure that treatments are effective and safe for all individuals. This requires targeted outreach and recruitment and adapting protocols to include transgender-specific considerations.
Time and Burden: Adding a clinical trial to existing healthcare appointments can be a burden, especially for TGI folks who may already face difficulties finding qualified providers
Data collection: Clinical trials should collect and report data on gender identity, and potentially other relevant demographic factors, to allow for accurate analysis of the safety and efficacy of treatments in transgender populations.
Cultural competency: Researchers and healthcare providers involved in clinical trials should receive education and training on transgender health issues, cultural competency, and understanding of the unique needs and experiences of transgender individuals.
Informed consent: Twenty eight percent of the TGI folks are outed without their consent. Informed consent processes should be tailored to the needs of transgender individuals, including providing information about any potential impacts of hormone therapy on trial outcomes.
Transgender-specific care: Clinical trials should provide transgender-specific care, such as hormone therapy or surgical care, when appropriate, and this care should be included in the trial protocols.

Transgender discrimination in clinical trials can limit the access of transgender individuals to potentially life-saving treatments and exacerbate existing health disparities. To address this issue, clinical trials must ensure the inclusion of transgender individuals, data collection, cultural competency, informed consent tailored to transgender individuals, and transgender-specific care when needed. These efforts can ensure that transgender individuals are included in clinical trials, receive the care they need, and improve health outcomes for all.
Fourth Pillar: Policymakers

Transgender policymakers are individuals who are part of the transgender community and hold positions of power or influence in policy-making processes. They may work at the local, state, or national level and be involved in developing policies related to healthcare, employment, education, housing, and other areas of social policy. Having transgender policymakers can be important for several reasons:
Advocacy: Transgender policymakers can be advocates for policies that advance the rights and interests of transgender individuals, such as policies that provide access to gender-affirming healthcare, protect against discrimination, and ensure equal opportunities in employment and education.
Role models: Transgender policymakers can serve as role models for other transgender individuals and inspire them to pursue leadership roles in their communities and policy-making.
Impact: Transgender policymakers can directly impact policies and legislation that affect the lives of transgender individuals. They can help to ensure that policies are inclusive, effective, and reflective of the needs and experiences of transgender individuals.
Exclusions: Policy-makers may exclude transgender individuals from certain healthcare services or health insurance coverage, such as gender-affirming care.
Limitations: Policy-makers may place limitations on access to healthcare services for transgender individuals, such as requiring extensive documentation to prove gender identity or imposing age limits for accessing hormone therapy.
Stigma and bias: Policy-makers may reinforce negative stereotypes or beliefs about transgender individuals, such as the belief that gender-affirming care is not medically necessary or is a form of cosmetic surgery.
Inadequate services: Policy-makers may not adequately address the unique healthcare needs of transgender individuals, such as providing insufficient mental health services or not providing access to gender-affirming care.
To address transgender discrimination in healthcare policy-making, several steps can be taken:
Representation: Transgender policymakers can bring a unique perspective to policy-making processes and ensure that the needs and experiences of transgender individuals are taken into account. This can help to ensure that policies are responsive to the needs of the community and address healthcare disparities.
Education: Policy-makers should receive education and training on transgender health issues, cultural competency, and anti-discrimination. This can help to dispel myths and stereotypes and ensure that policies are based on accurate information and evidence.
Research and data collection: Policy-makers should prioritize research and data collection efforts to identify healthcare disparities and barriers to care for transgender individuals. This can help to inform policy-making and ensure that policies are responsive to the needs of transgender individuals.
Legal protections: Policy-makers should establish legal protections to prohibit discrimination in healthcare policies. This can include measures such as bans on discriminatory exclusions or limitations, clear guidance on providing healthcare to transgender individuals, and effective enforcement mechanisms.
Community engagement: Policy-makers should engage with transgender individuals and community-based organizations to ensure that policies are developed and implemented in a way that meets the needs of the community.
There is a list of bills across statehouses, including drag performance bans, bathroom usage restrictions, limits on LGBTQ discussions in schools, and obstacles to changing the gender marker on a driver’s license or birth certificate. However, the rising age minimums proposed to access gender-affirming care is majorly concerning.
Transgender policymakers can play a critical role in advancing the rights and interests of transgender individuals and addressing healthcare disparities. By providing representation, advocacy, education, role models, and impact, they can help to ensure that policies are responsive to the needs of the community and promote equality and social justice.
In conclusion, creating a supportive community is vital to improving healthcare equity for transgender individuals. Community-based organizations can provide critical support to transgender individuals, including access to healthcare, legal resources, and support groups. These organizations can also advocate for policy changes and provide education and training to healthcare providers. By building a supportive community, transgender individuals can access the resources and care they need to improve their health outcomes.
Here are some resources for you.
Here are a few organizations that help in advancing clinical trials and humanizing healthcare. Rebekon Consulting LLC has partnered with SGM Alliance in this fight for health equity.
Celia Sandhya Daniels, Founder and CEO of Rebekon Consulting LLC can be contacted through LinkedIn or celia@rebekon.com




Comments